In today's value-based healthcare landscape, patient satisfaction scores are more than just a metric; they are a critical indicator of quality, a driver of reimbursement, and a cornerstone of a provider's reputation. High scores directly correlate with better patient outcomes, increased loyalty, and a stronger bottom line, making the pursuit of patient satisfaction a strategic imperative for any modern clinic, hospital, or healthcare system. Moving beyond generic advice, this guide offers a deep dive into 10 practical, evidence-based strategies that organizations can implement to meaningfully improve patient satisfaction scores.
We'll explore everything from optimizing operational workflows with smart technology to fostering a culture of empathy through targeted staff training. As healthcare providers increasingly recognize the imperative of patient satisfaction, it's crucial to consider broader systemic changes; for example, exploring the digital transformation's role in the future of European healthcare highlights how larger trends impact individual patient experiences.
This article provides actionable steps, real-world examples, and key metrics to guide your efforts. Whether you're aiming to boost HCAHPS scores, enhance your online reputation, or simply build a more patient-centric practice, these proven methods will provide a clear roadmap to achieving tangible, lasting results.
1. Implementing Comprehensive Patient Communication Protocols
Effective communication is the cornerstone of a positive patient experience and a key driver to improve patient satisfaction scores. This strategy involves creating a structured system for clear, timely, and empathetic dialogue at every stage of the care journey. It moves beyond simple appointment reminders to build a comprehensive framework that includes pre-visit instructions, real-time updates on wait times, post-visit follow-ups, and accessible channels for patient questions.

This approach reduces patient anxiety by setting clear expectations and demonstrates that your practice values their time and concerns. For example, Mayo Clinic utilizes an advanced patient portal and SMS system to keep patients informed, while Kaiser Permanente's integrated platform ensures seamless communication across departments.
Actionable Steps for Implementation
- Automate Routine Communications: Use automated systems for appointment confirmations, reminders, and post-visit surveys. This frees up staff to handle more complex patient needs. For instance, a virtual medical receptionist can manage scheduling and answer routine questions 24/7.
- Offer Preferred Channels: Allow patients to opt-in for their preferred communication method, whether it's email, SMS, phone calls, or a patient portal.
- Train Staff on Empathy: Equip your team with empathetic communication techniques to handle sensitive conversations and de-escalate patient frustrations effectively.
- Gather Feedback: Regularly survey patients specifically about the clarity and timeliness of your communication to identify and address any gaps.
2. Reducing Wait Times Through Operational Efficiency
Excessive wait times are a primary source of patient frustration and can significantly lower satisfaction ratings. To improve patient satisfaction scores, healthcare providers must focus on operational efficiency by re-engineering workflows to minimize delays. This involves a strategic approach to appointment scheduling, check-in processes, and patient flow management, ensuring that every minute of a patient's time is respected from arrival to departure.
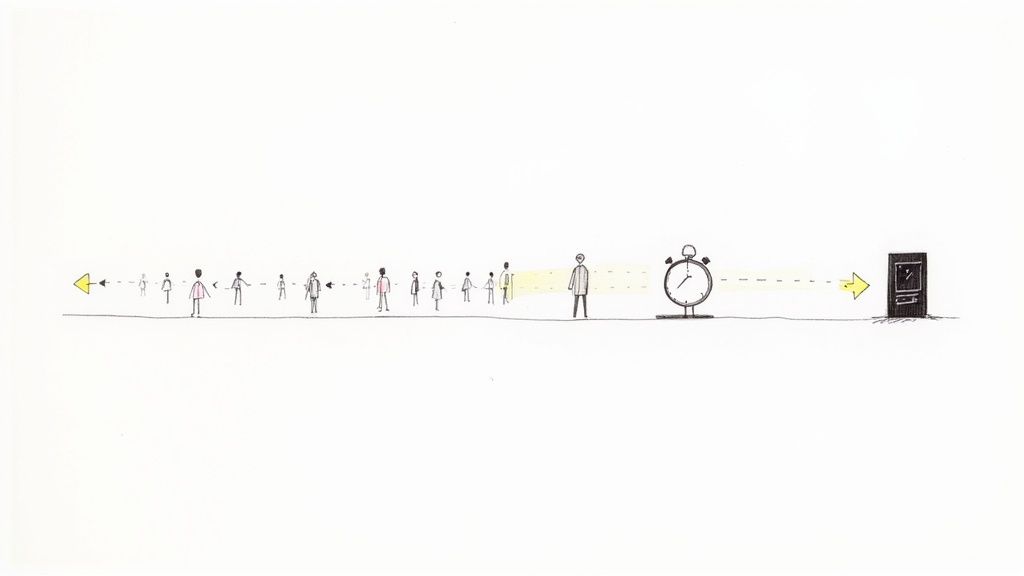
This strategy directly tackles one of the most visible and frustrating aspects of the patient journey. For instance, many urgent care centers display real-time wait times on digital boards, managing expectations transparently, while the Veterans Health Administration has launched initiatives using lean management principles to streamline processes and cut down appointment backlogs.
Actionable Steps for Implementation
- Analyze and Optimize Patient Flow: Use data analytics to map the entire patient journey and identify specific bottlenecks, whether at check-in, in the exam room, or during checkout.
- Implement Smart Scheduling: Stagger appointment times based on visit type and complexity rather than using uniform 15-minute slots. An advanced medical appointment scheduling software can automate this process to optimize provider utilization.
- Involve Frontline Staff: Engage your receptionists, nurses, and medical assistants in brainstorming solutions. They often have the most practical insights into day-to-day operational hurdles.
- Create Fast-Track Pathways: Develop dedicated, streamlined processes for simple, routine visits like follow-ups or injections to prevent them from getting stuck behind more complex cases.
3. Developing Person-Centered Care Plans
Person-centered care shifts the focus from treating a condition to caring for an individual, which is a powerful way to improve patient satisfaction scores. This strategy involves creating individualized care plans that integrate a patient's personal values, preferences, cultural background, and life goals. By actively involving patients in shared decision-making, you empower them as partners in their own health, demonstrating that they are respected as unique individuals, not just a collection of symptoms.
This collaborative approach fosters trust and improves adherence to treatment plans, leading to better outcomes and higher satisfaction. For example, the VA Healthcare system utilizes a patient-centered medical home model that coordinates care around the patient's specific needs, while Geisinger Health System has pioneered care coordination that ensures every aspect of a patient's treatment aligns with their personal goals.
Actionable Steps for Implementation
- Use Patient Preference Tools: Implement standardized assessment tools to systematically gather information about what matters most to your patients beyond their clinical diagnosis.
- Train in Motivational Interviewing: Equip providers with motivational interviewing skills to help patients articulate their own goals and motivations for getting well, fostering a collaborative spirit.
- Document Goals Explicitly: Make patient goals a prominent and explicit part of the electronic medical record, ensuring the entire care team is aligned with the patient's priorities.
- Revisit Plans Regularly: Schedule regular check-ins to review and update the care plan, ensuring it remains relevant as the patient's condition, goals, or life circumstances change.
4. Enhancing Physical Environment and Amenities
The physical environment of a healthcare facility is a patient's first tangible impression and plays a crucial role in their overall experience. A welcoming, clean, and comfortable setting can significantly reduce patient stress and anxiety, which is a powerful way to improve patient satisfaction scores. This strategy focuses on optimizing the facility's atmosphere, from the waiting room to the exam room, by considering elements like cleanliness, comfort, clear navigation, and thoughtful amenities that signal a commitment to patient well-being.

A positive physical space makes patients feel valued and cared for even before they see a clinician. For example, Mayo Clinic is renowned for its patient-centered facility design, incorporating natural light, art, and intuitive layouts. Similarly, Cleveland Clinic focuses on creating patient-friendly lobbies and waiting areas with comfortable seating and amenities, transforming a potentially stressful wait into a more pleasant experience.
Actionable Steps for Implementation
- Conduct Facility Audits: Regularly walk through your facility from a patient's perspective to identify areas for improvement, such as outdated decor, uncomfortable furniture, or poor signage.
- Invest in Comfort and Cleanliness: Ensure waiting areas are impeccably clean and offer comfortable seating, complimentary Wi-Fi, and refreshments. Simple touches like accessible hand sanitizer stations and tissues show attention to detail.
- Use Calming Design Elements: Incorporate calming colors, artwork, and natural elements like plants to create a soothing ambiance. Maximizing natural light can also have a profoundly positive impact on mood.
- Ensure Clear Navigation and Accessibility: Implement clear, easy-to-read signage to help patients navigate your facility with ease. Ensure full accessibility for patients with disabilities, including ramps, automatic doors, and accessible restrooms.
5. Implementing Staff Training and Cultural Competence Programs
A well-trained, culturally competent team is fundamental to providing exceptional care and is a powerful lever to improve patient satisfaction scores. This strategy focuses on developing comprehensive training programs that go beyond clinical skills to include professional communication, empathy, and cultural awareness. When staff understand the diverse backgrounds of their patients, they can communicate with greater respect and sensitivity, which directly impacts the patient's experience and perception of care.
This approach ensures that every patient feels seen, heard, and respected, regardless of their background. For example, Cleveland Clinic mandates cultural competence training for all caregivers to address the needs of its diverse patient population, while Johns Hopkins Medicine’s diversity initiatives are integrated into every aspect of its operations, from hiring to patient interaction.
Actionable Steps for Implementation
- Mandate Regular Training: Make training in empathy, diversity, and patient service a mandatory and recurring requirement for all staff, not just a one-time onboarding session.
- Utilize Realistic Scenarios: Incorporate role-playing and real-world case studies into training sessions to help staff practice navigating difficult or culturally sensitive conversations.
- Tie Training to Performance: Link the principles taught in training to staff performance evaluations and professional development goals to create clear accountability for behavioral change.
- Gather Feedback and Evolve: Continuously collect feedback from both staff and patients on their experiences to refine and improve the training programs over time, ensuring they remain relevant and effective.
6. Establishing Effective Complaint Resolution and Feedback Systems
A proactive approach to patient feedback is crucial to improve patient satisfaction scores. This strategy involves creating accessible and transparent systems for patients to voice concerns and file complaints, coupled with a clear, efficient resolution process. By demonstrating responsiveness, healthcare providers show they value patient input and are committed to continuous improvement. Patients who feel their concerns are heard and acted upon often report higher satisfaction, even if their experience began with a problem.
This system transforms negative experiences into opportunities for growth and loyalty. For instance, many hospital networks now employ dedicated patient advocates whose sole function is to investigate and resolve patient issues. Similarly, initiatives from organizations like The Leapfrog Group encourage formal feedback mechanisms as part of their safety and quality ratings, highlighting the industry-wide importance of listening to the patient's voice.
Actionable Steps for Implementation
- Respond Promptly: Acknowledge all complaints within 24-48 hours to show patients their feedback is being taken seriously. A timely response prevents frustration from escalating.
- Empower Front-Line Staff: Train and authorize front-line employees to resolve minor issues on the spot. This immediate action can often de-escalate a situation before it becomes a formal complaint. For more complex interactions, discover techniques for how to handle customer complaints effectively.
- Systematically Document and Analyze: Use a centralized system to log all feedback and complaints. Perform quarterly trend analyses to identify recurring problems and systemic issues that need addressing.
- Close the Loop: Always follow up with the patient to inform them of the actions taken based on their feedback. This final step confirms their complaint was resolved and demonstrates accountability.
7. Leveraging Patient Portals and Digital Health Tools
Empowering patients with digital access to their health information is a powerful strategy to improve patient satisfaction scores. This involves implementing secure patient portals and digital health tools that give patients autonomy over their care. These platforms allow individuals to view medical records, schedule appointments, request prescription refills, and communicate directly with providers, offering a level of convenience and control that modern consumers expect.

This approach not only enhances patient engagement but also streamlines administrative workflows, reducing staff burden and operational costs. For example, the VA's MyHealtheVet portal and widely used systems like Epic's MyChart have demonstrated how providing direct access to test results and secure messaging can significantly boost patient involvement and satisfaction by making healthcare more transparent and accessible.
Actionable Steps for Implementation
- Prioritize User Experience: Design or choose a patient portal that is intuitive, mobile-friendly, and easy to navigate. A complex interface will deter adoption and lead to frustration.
- Provide Robust Support: Offer comprehensive training materials, tutorials, and a dedicated helpdesk to assist patients who are less tech-savvy.
- Set Clear Communication Expectations: Establish and clearly communicate expected response times for messages sent through the portal to manage patient expectations effectively.
- Integrate Automation: Use digital tools to handle routine inquiries and tasks, which can drastically improve efficiency. Discover how to automate customer service to free up your team for more complex patient needs.
- Ensure Data Security: Implement stringent cybersecurity measures to protect sensitive patient data and build trust in your digital platforms.
8. Creating Patient Education and Health Literacy Programs
Empowering patients through knowledge is a powerful way to improve patient satisfaction scores. This strategy focuses on developing accessible, evidence-based education programs that help patients understand their conditions, treatment options, and self-management strategies. When patients are well-informed, they feel more in control of their health, leading to better adherence, improved outcomes, and a stronger partnership with their care providers.
Higher health literacy directly correlates with higher satisfaction because it reduces confusion and anxiety. For instance, Cleveland Clinic maintains a comprehensive online health library with easy-to-understand articles and videos, while Stanford Medicine's health literacy initiatives ensure all patient materials are clear and actionable. This proactive educational approach builds trust and demonstrates a deep commitment to patient well-being beyond the clinic walls.
Actionable Steps for Implementation
- Simplify Your Language: Write all patient-facing materials at an 8th-grade reading level. Use plain language, avoid medical jargon, and focus on the most critical information.
- Utilize Visual Aids: Incorporate infographics, charts, and videos to explain complex concepts. Visual information is often easier to process and remember than text alone.
- Provide Multilingual Resources: Offer key educational materials in the top languages spoken by your patient population to ensure equitable access to information.
- Use the "Teach-Back" Method: After explaining a concept, ask patients to describe it back to you in their own words. This simple technique confirms their understanding and identifies any areas needing clarification.
9. Implementing Provider-Patient Relationship and Continuity of Care
Establishing a consistent relationship between a patient and their care team is fundamental to improve patient satisfaction scores. This strategy focuses on continuity of care, ensuring patients see the same provider or a coordinated team consistently, which reduces fragmentation and builds trust. When patients feel known and understood by their healthcare providers, their confidence in the care they receive increases significantly.
This approach minimizes the need for patients to repeat their medical history, leading to more efficient and personalized consultations. For example, the Patient-Centered Medical Home (PCMH) model and the Veterans Health Administration’s programs prioritize assigning patients to a specific provider team to foster long-term therapeutic relationships, resulting in better health outcomes and higher satisfaction.
Actionable Steps for Implementation
- Assign Patients to a Primary Provider: Implement panel management where each patient is assigned to a specific primary care provider or a small, dedicated care team to ensure consistency.
- Facilitate Warm Handoffs: When a specialist referral is needed, ensure the primary provider personally introduces the patient to the specialist, either in person or via a coordinated call, to maintain a seamless care experience.
- Utilize Team Huddles: Start each day with a brief team meeting to discuss complex patient cases and coordinate care plans, ensuring all team members are aligned.
- Create Clear Transition Protocols: Develop standardized protocols for documenting and communicating during transitions of care, such as from hospital to home, to prevent information gaps and medical errors.
10. Measuring and Using Patient Satisfaction Data for Continuous Improvement
To truly improve patient satisfaction scores, you must move from guessing what patients want to knowing what they need. This strategy involves systematically collecting feedback through validated surveys like HCAHPS or Press Ganey, analyzing the results to identify trends, and using those data-driven insights to implement specific, targeted improvements. It creates a continuous feedback loop where patient voices directly shape operational and clinical enhancements, ensuring that changes are meaningful and effective.
This data-centric approach transforms patient satisfaction from a vague goal into a measurable objective. For example, Cleveland Clinic uses an integrated dashboard to monitor patient feedback in real-time, allowing department heads to quickly address issues. Similarly, the CMS STAR Ratings for health plans rely heavily on patient satisfaction data, directly linking quality of care to measurable outcomes and creating accountability.
Actionable Steps for Implementation
- Implement Diverse Measurement Methods: Don't rely solely on one survey. Combine quantitative data from surveys with qualitative insights from patient interviews or focus groups. Explore various customer satisfaction measurement methods to get a complete picture.
- Create Actionable Dashboards: Translate raw data into visual, easy-to-understand dashboards for staff and leadership. Highlight key performance indicators and pinpoint specific areas, like wait times or staff communication, that need attention.
- Share Results Transparently: Foster a culture of accountability by sharing satisfaction data across all departments. When staff understand the "why" behind new initiatives, they are more likely to support them.
- Close the Feedback Loop: Use the data to make specific changes, and then measure the impact of those changes. Robust outcome evaluation methods are essential for accurately assessing the success of your patient satisfaction initiatives.
Patient Satisfaction: 10-Strategy Comparison
| Initiative | 🔄 Implementation Complexity | ⚡ Resource Requirements & Efficiency | 📊 Expected Outcomes (Impact) | 💡 Ideal Use Cases | ⭐ Key Advantages |
|---|---|---|---|---|---|
| Implementing Comprehensive Patient Communication Protocols | 🔄🔄 Medium — multi-channel setup & training | ⚡⚡ Low–Moderate resources; automation boosts efficiency | ⭐⭐⭐⭐ Reduced anxiety, fewer no-shows, better coordination | Ambulatory care, high-volume clinics, pre/post‑visit workflows | Lower no-shows; improved adherence; stronger patient trust |
| Reducing Wait Times Through Operational Efficiency | 🔄🔄🔄 High — process redesign and scheduling overhaul | ⚡⚡⚡ Moderate–High tech & change management; large throughput gains | ⭐⭐⭐⭐ Faster service, higher satisfaction, improved productivity | Emergency departments, urgent care, busy outpatient centers | Increased throughput; clearer patient flow; measurable time savings |
| Developing Person-Centered Care Plans | 🔄🔄🔄 Medium–High — individualized planning & training | ⚡⚡ Moderate resources; time‑intensive planning | ⭐⭐⭐⭐ Higher engagement, adherence, and clinical outcomes | Chronic disease management, primary care, complex patients | Aligns care with values; improves adherence and satisfaction |
| Enhancing Physical Environment and Amenities | 🔄🔄 Medium — design and construction projects | ⚡ Low efficiency gain vs high capital/maintenance cost | ⭐⭐⭐ Immediate perception and comfort improvements; variable clinical impact | Hospitals, clinics focused on brand/retention, patient-facing spaces | Strong first impressions; reduced anxiety; competitive advantage |
| Implementing Staff Training and Cultural Competence Programs | 🔄🔄 Medium — curriculum + ongoing reinforcement | ⚡⚡ Moderate ongoing investment; improves interaction efficiency | ⭐⭐⭐⭐ Better patient interactions, fewer complaints, improved equity | Diverse patient populations, institutions with experience gaps | Reduces disparities; improves communication and staff morale |
| Establishing Effective Complaint Resolution and Feedback Systems | 🔄🔄 Medium — workflow, staff roles, and tracking | ⚡⚡ Moderate staffing; time‑intensive but yields actionable data | ⭐⭐⭐⭐ Builds trust, identifies issues, prevents escalation | Organizations aiming for continuous improvement and risk reduction | Rapid detection of problems; closes the loop with patients |
| Leveraging Patient Portals and Digital Health Tools | 🔄🔄🔄 High — IT integration, security, interoperability | ⚡⚡ High upfront cost; increases convenience and access (24/7) | ⭐⭐⭐⭐ Improved access, adherence, and remote monitoring | Tech‑savvy populations, chronic disease programs, telehealth services | Self-service access; reduces admin calls; supports remote care |
| Creating Patient Education and Health Literacy Programs | 🔄🔄 Medium — content development and tailoring | ⚡⚡ Moderate resources for development and updates | ⭐⭐⭐⭐ Improved understanding, adherence, and outcomes | Pre/post‑op, chronic care, populations with low health literacy | Empowers patients; reduces readmissions; supports informed decisions |
| Implementing Provider‑Patient Relationship & Continuity of Care | 🔄🔄🔄 High — scheduling, panel management, coordination | ⚡⚡ Moderate system and staffing investment; long‑term efficiency | ⭐⭐⭐⭐ Greater trust, fewer duplications, better outcomes | Primary care, PCMH models, long‑term chronic care management | Strong continuity; improved preventive care and trust |
| Measuring & Using Patient Satisfaction Data for Continuous Improvement | 🔄🔄 Medium — survey systems, dashboards, accountability | ⚡⚡ Moderate resources for measurement & analytics | ⭐⭐⭐⭐ Targeted improvements, accountability, measurable change | Systems pursuing CQI, benchmarking, and performance management | Data-driven prioritization; tracks impact and guides interventions |
From Metrics to Mission: Integrating Patient Satisfaction into Your Core Strategy
The journey to improve patient satisfaction scores is far more than an exercise in data collection or a box-ticking requirement. As we've explored, it represents a fundamental shift from a provider-centric model to a patient-centered mission. True, lasting improvement is not achieved by implementing a single strategy but by weaving a consistent thread of empathy, efficiency, and empowerment through every facet of your organization.
From establishing robust communication protocols and leveraging digital tools to reducing wait times and fostering a culture of continuous feedback, each strategy serves as a vital pillar supporting a superior patient experience. The key is to move beyond viewing these as isolated tasks and instead see them as interconnected components of a holistic system designed around the patient’s needs and preferences.
Key Takeaways for Lasting Impact
The most crucial insight is that patient satisfaction is not a lagging indicator of past performance; it is a leading driver of future success. It directly influences clinical outcomes, patient loyalty, and your organization's reputation.
- Embrace a Proactive Stance: Don't wait for negative feedback. Proactively seek out opportunities for improvement by analyzing wait times, streamlining digital access, and training staff to anticipate patient needs.
- Technology as an Enabler, Not a Replacement: Tools like patient portals and AI-powered communication systems should enhance human connection, not replace it. Use them to free up your staff to focus on high-value, empathetic interactions.
- Consistency is Crucial: A single positive interaction is easily undone by a frustrating phone call or a long, unexplained wait. Every touchpoint, from the initial appointment booking to the follow-up call, must reflect your commitment to patient-centered care.
Your Actionable Next Steps
Transforming these concepts into reality requires a deliberate, step-by-step approach. Begin by selecting one or two high-impact areas discussed in this article, such as refining your feedback collection process or overhauling your appointment scheduling system. Set clear, measurable goals and empower a dedicated team to lead the change.
By consistently demonstrating that you value patients as active partners in their health journey, you do more than just improve patient satisfaction scores. You build a foundation of trust and loyalty that strengthens your practice, enhances clinical effectiveness, and solidifies your role as a truly patient-first healthcare provider. This commitment is the ultimate metric of success, turning a simple score into a powerful statement about your organization's core values.
Ready to transform your front desk and ensure no patient call goes unanswered? See how Marlie Ai can automate appointment scheduling, answer common questions, and free up your staff to focus on in-person care. Discover the future of patient communication at Marlie Ai.

